Author: Tim Scott, Head of Sales (retired), Condair Ltd

Read the original article as published in Energy in Buildings & Industry Oct 2016
Humidification for health – is it worth the energy?
The optimum level of humidity is a determining factor in the success of many manufacturing processes, such as textiles and printing, as well as playing a vital role in our general health and well-being. As humidification specialists, rarely do we see humidifiers being turned off to save energy in manufacturing facilities, as there would be an immediate and obvious effect on the production line. However, we often see humidification being sacrificed for energy savings when it comes to humidity control for the health and well-being of people.
So when it comes to balancing the need to save energy against humidity control for human health, how do the arguments stack-up?
Given that it requires around 0.75kW to turn one kilo of water to steam and an average London office accommodating around 250 staff could need approximately 80,000kg of steam humidification over the course of a year, it is clear that humidification can place a burden on the energy demands of a building. However, what isn’t so obvious is the effect turning off the humidifiers has on the building’s occupants or on the business itself. The detrimental effects of exposure to dry air occur over time and unlike temperature, a dry atmosphere isn’t as immediately noticeable as a particularly cold or hot environment.
If the correlation between exposure to dry air and the effect it has on health was more evident, with the resulting increase in absenteeism recognised, the energy savings from not humidifying wouldn’t be so attractive to a business.
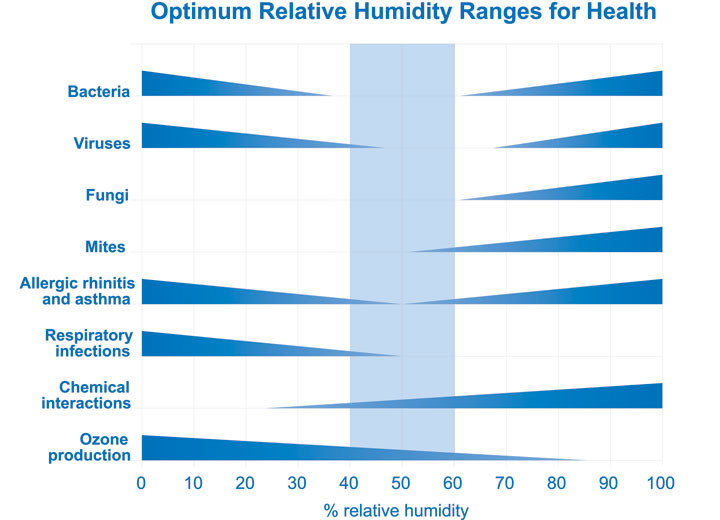
In 1985 Sterling et al examined all the scientific evidence for how humidity affects the growth and survival rates of many elements that pose a risk to human health. This included bacteria, viruses, mould, dust mites, ozone and others. The humidity levels at which these elements presented the greatest and least risk to human health were plotted on the “Sterling Chart”. It showed the optimum level to reduce the risk to health from these elements to be between 40-60%RH, a figure also supported by many other studies since.
In a more recent article published in the Journal of Infection, Jane Metz and Adam Finn, of the University of Bristol, reviewed all research specfically associated to humidity and winter-time influenza peaks. They concluded that low humidity was a key casual factor in the spread of flu and that artificially increasing humidity in public places was “an exciting and novel potential strategy for disarming flu.”
Alongside the sustaining effects dry air has on airborne pollutants, it also directly effects on our bodies. Dry air has been shown to draw moisture from us resulting in dehydration and drying of the skin and mucous membranes in the nose and throat, which is one of our body’s main defences against airborne contaminants.
The Sterling Chart - showed the optimum level to reduce the risk to health from these elements to be between 40-60%RH, a figure also supported by many other studies since.
So as well as being a proven conduit for airborne infection and the spread of viruses, dry air below 40%RH impairs our ability to fight off these external threats. Long term exposure to dry air therefore must increase the risk of ill-health through airborne infections, such as colds and flu, with a resulting increase in workplace absenteeism.
The Chartered Institute of Personnel and Development (CIPD) in its 2015 report on workplace absence found that in the UK the average level of employee absence is 6.9 days per year. The main reason reported for absence is minor short term illnesses, such as colds and flu. The CIPD estimate this costs employers £554 per employee per year. Reducing the spread of colds and flu should be a priority for any employer wanting to reduce absenteeism and improve employee well-being. Correct environmental control, including maintaining the humidity at between 40-60%RH, will help achieve this goal.
So rather than turning off the humidification system and ignoring the very real, but sometimes neglected, need for humidity control, can building operators save energy without risking the health of employees and the public?
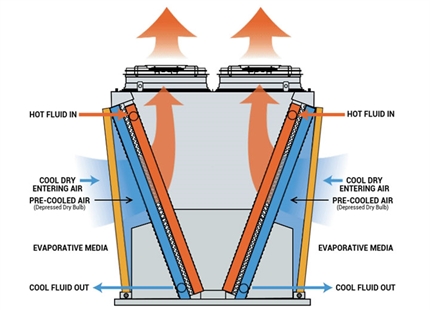
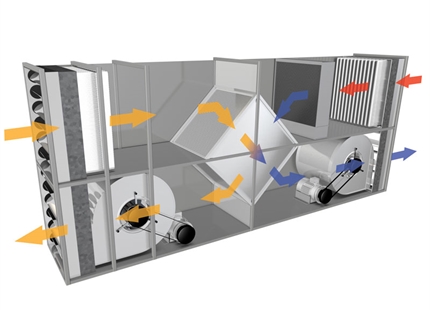
The typical office humidification system in the UK uses electrically generated steam humidifiers. However, there are alternatives to this technology that evaporate or spray water, either in a centrally ducted air conditioning system or directly into a room. For our average London office, using an equivalent evaporative humidifier rather than steam could mean a reduction in energy cost of around two thirds.
If replacing an existing steam system isn’t viable, modifications can be made that could improve energy consumption. For instance, using an RO water filter to remove minerals from the supply water would eliminate the need for regular drainage of hot water to control mineral build-up in the humidifier’s water tank. Regular servicing can also improve the energy efficiency of a steam humidifier and reduce its running cost.
Examining the hours of operation can identify potential opportunities to reduce the energy consumption of a humidification system without sacrificing a building’s humidity control and dropping below the 40%RH needed for human health and well being.
Without humidification, internal humidity in our average London office could drop below 40%RH from mid-October through to May with the driest months being the coldest, from December to February. It’s no co-incidence that this is also the time that seasonal flu is most prevalent across the country. If the relationship between illness, workplace absence and low humidity was as obvious to perceive as the relationship between a textile factory’s air humidity and the final weight of its product, not controlling humidity to save energy would never be a consideration.