
Low humidity and its effects on airborne infection
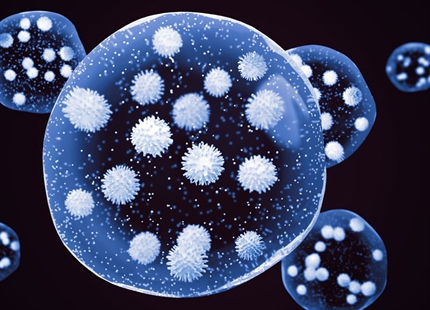
Everyone releases tiny water droplets, called aerosols, when they breath, talk, cough or sneeze. The microscopic droplets are composed of around 97% water and 3% solutes - salts, proteins and numerous other substances.
Under normal circumstance, this personal contribution to the "air we share" has no negative effect on us. However, when a person has respiratory viral or bacterial infection, their exhaled air will contain harmful, contagious microbes. Once emitted into the air, these harmful microbes can infect other people, either by direct inhalation or through deposition on to a surface and subsequent touch contact.
The humidity of air is a major factor in the transmission of airborne microbes.
In dry atmospheres below 40%RH expelled droplets rapidly lose their moisture content through evaporation. As smaller droplets remain airborne for longer, this evaporation results in more droplets capable of staying airborne and increases the overall time they can float around.
The droplet's water loss also changes its structure to a crystallized solid state. Viruses and bacteria get preserved in a floating capsule, where they remain infectious and have a greater potential to infect other people.
In an atmosphere above 40%RH, expelled droplets retain their moisture content, are heavier and less able to remain airborne. Furthermore, the dissolved salts inside the remaining airborne droplets create a hostile environment for any suspended microbes, decreasing their infectious nature and any risk they pose to health.
A humidity above 40%RH combats airborne infection by reducing the quantity of microbes in the air and inhibiting their infectious capability.

Droplets less than 4 microns expelled during breathing, speaking, coughing or sneezing can remain airborne and infectious for hours.
In humidity above 40% supersaturated solutes in the infectious aerosols inactivate the microbes and protect us from infections. The water containing droplets settle faster and have shorter "floating time" than in lower humidity atmospheres.
Below 40%RH infectious droplets lose their water content and become “dry aerosols”. Microbes get incorporated in the dry structures of the solutes, are preserved and remain infectious for longer. "Floating time" and the number of microbes is increased, compared to atmospheres with a humidity greater than 40%RH.
Scientific evidence relating to humidity and airborne infection

Parhizkar et al 2022

Jennifer M. Reiman et al 2018
Dietz L. et al 2020
Casanova LM et al 2010

Koep T et al 2013

Alsmo T, Alsmo C 2016
Yang W et al 2012

Dunklin EW, Puck TT 1948

Shaman J et al 2010
